More than ever, people are interested in applying the practical advice that emerges from scientific research on exercise and the immune system.
If you…
- Choose foods with antioxidants
- Try to get lots of sleep
- Eat plenty of whole foods
- Try to eat a plant-based diet
- Prioritize mental health as a pillar of overall health
- Take “immune-boosting” supplements…
…then you have been applying the conclusions of immune research to your life.
But, what about exercise? Can exercise be part of your strategy to stay healthy and fight off illness?
The answer isn’t as straightforward as you might think.
Even though regular exercise is necessary for overall health, the question about the impact of exercise on the immune system in the short and long term has been the subject of scientific research for decades.
The answers to the questions above have varied, depending on factors like exercise intensity, levels of fatigue, and physical fitness.
In this article, not only will you find out how exercise impacts the immune system, but you’ll also learn some of the research-backed principles to follow for your exercise routine to be part of your immune-health strategies.
Refresher: What Makes Up the Immune System?
The immune system is responsible for keeping us healthy by protecting our bodies from bacteria, viruses, fungi, and toxins.
The immune system is an all-encompassing system that involves cells and organs that are important parts of other systems. It also requires nutrients and components that are stored in other organs for healthy function. Ultimately, the immune system is the epitome of how our entire body is interconnected, and how a misbalance in one specific system can affect the entire body.
Any action on the body has the potential to trigger an immune system response if cells are stressed, damaged, or if external bodies are introduced into your body.
Some of these external actions that can cause the immune system to respond include:
- The environment, if there are allergens, like pollen, mites, and dander; toxins, like heavy metals or residual chemicals; or other stressors in the environment.
- Exposure to pathogens, which can be found in the air we breathe, the food we eat, and transferred to you by other people, directly or indirectly.
- In addition to exercise, which is discussed below, other lifestyle choices, including sleep, diet, and smoking. While a balanced diet rich in healthy fats, lean proteins, fruits, and vegetables is important for immune system health, other actions, like smoking, are detrimental to health. There is ample evidence that shows how smoking and second-hand smoke negatively impacts your immune system response, as well as how eating a diet high in ultra-processed foods can trigger an inflammatory response and is linked to disease.
The way to measure immune system health is by looking at the cells that fight off infections and inflammation.
Immune system cells include:
- White blood cells (leukocytes), which refer to a category of cells that identify and eliminate pathogens (potentially damaging invaders). They include phagocytes, mast cells, eosinophils, basophils, and natural killer (NK) cells.
- Phagocytes, which include neutrophils, macrophages, and dendritic cells that travel throughout the body in pursuit of invading pathogens and produce chemicals that activate different responses. Neutrophils travel in the bloodstream, and macrophages are found in tissues. Dendritic cells are phagocytes found on the skin that link the bodily tissues to the immune system.
- Mast cells, which are found in connective tissues and mucous membranes and regulate inflammation. The degranulation of mast cells is what is responsible for allergic reactions, which is what occurs when the immune system overreacts to non-pathogenic substances.
- Basophils and eosinophils, which secrete chemical mediators that defend the body against parasites and play a role in the allergic response.
- Lymphocytes, which include B cells and T cells, which are produced by specialized cells in the bone marrow.
- The T cells recognize pathogens that have been processed and include the killer T cells, which kills dysfunctional cells or those infected with viruses, and helper T cells, which help determine how the body should respond to a particular pathogen.
- The B cells represent the body’s antibodies or the body’s acquired defense system. They include antigen-specific receptors that recognize specific pathogens without the need for processing them. There are different B cells for different pathogens.
The cells above have to be produced and stored somewhere. Some of the organs involved in the immune system include:
- Adenoids, which are located at the back of the nasal passage
- Bone marrow, which produces immune cells
- Lymph nodes, which also produce immune cells and are located throughout the body
- Lymphatic vessels, which carried lymphocytes throughout the body through the bloodstream
- Peyer’s patches, which are lymph nodes in the small intestine
- Spleen, which is an organ in the abdomen that contains white blood cells and components that promote fluid balance in the body
- Thymus, which is a specialized lymphoid where lymphocytes (T cells) are matured
- Tonsils, which are the masses you can see at either side of the beginning of the throat and produce white blood cells and antibodies
Ultimately, since every part of the body needs protection from outside invaders, there is not one part of the body that doesn’t depend on our immune system function for its health.

Learn How to Become an AFPA Autoimmune Holistic Nutrition Specialist in Less Than 6 Months
Become an expert in helping people living with an autoimmune disease feel better.
Example: Food Allergies and Immune Response
Let’s look more closely at an example to get a clearer idea of how the immune system responds to a threat.
Food allergies are very common, and they are a good example that illustrates the immune response.
Some people have an overactive immune system that responds to certain components in foods as if they were pathogens. Depending on the type of food allergy, different mechanisms of action can be activated.
One of the most serious kinds of food allergies is that which is mediated by the antibody Immunoglobulin E (IgE). If a person has a high level of IgE, it could indicate a food allergy.
The immune system’s activation to an allergen can be divided into two phases: sensitization and then the allergic reaction. The process is broken down as follows:
- Chemicals of an allergen, like peanuts, are detected by a dendritic cell, a type of phagocyte. This activates the response of an allergen-specific T cell.
- The allergen-specific T cell recognizes the chemical as an allergen, and it then communicates with the helper T cell, which determines how the body should respond to the pathogen.
- The helper T cell sends interleukins, which are produced by mast cells, to B cells.
- The B cells activate allergen-specific IgE, which then bond to mast cells.
- The IgE on mast cells bond to the allergenic chemical in a food and spark the production of histamines, leukotrienes, cytokines, prostaglandins, and PAF. All of these chemicals initiate an allergic reaction.
- An allergic reaction can present itself as local symptoms, like swelling, itching, nausea, vomiting, and diarrhea, and systemic symptoms, like airway obstruction, hives, blood pressure drop, and arrhythmia.
The example above describes only one immune system pathway. The immune system responds to multiple other triggers that are not allergens, like diet, sleep, toxins in the environment, and, yes, exercise.
How the Immune System Responds to Exercise
But how about exercise? Hundreds of researchers dedicate their professional lives to answering the questions around the impact of exercise on the immune system through a field called sports immunology.
Here are some of the key research findings that link exercise to the immune system response:
- Exercise can either stimulate or reduce a stress response. Stress responses have inflammatory actions, and they stimulate the production and release of immune cells. Stress is modulated by several hormones and proteins, including cortisol, and it results in an inflammatory response, demonstrating that the body feels like it is threatened. Whether it stimulates or reduces the stress response depends on the mode, intensity, duration, and chronicity (how often) of exercise.
- Exercise influences our natural immunity, which is that with which we were born. It impacts T-cell and B-cell functions and cytokine responses through changes in blood circulation and the secretion of stress hormones. How exercise influences natural immunity also depends on the intensity, duration, and chronicity of exercise.
- Exhaustive exercise increases the production of free radicals, which can be a sign of damage to muscle cells. The degree of oxidative stress on the body depends on the degree of exhaustion of the person who performs the exercise.
- Moderate exercise has a protective effect on the immune system, whereas repeated bouts of strenuous exercise can result in immune dysfunction. Remember that what feels strenuous for an athlete is very different than what feels strenuous for a sedentary person.
- Regarding acute illnesses like the flu and bacterial infections, moderate exercise can help strengthen the immune system to fight illness. Researchers do not know exactly how exercise can increase immunity. They do propose several theories, including an increase in air circulation in and out of the lungs, which may help to flush out bacteria, and increased readiness to scavenge pathogens thanks to the acute inflammatory responses, or a reduction in circulating stress hormones.
What does this research tell us?
Exercise has a variable effect on the immune system.
The response to exercise varies greatly depending on factors that are related to your personal health status and factors related to the exercise you perform, specifically. We mention some of the factors below.
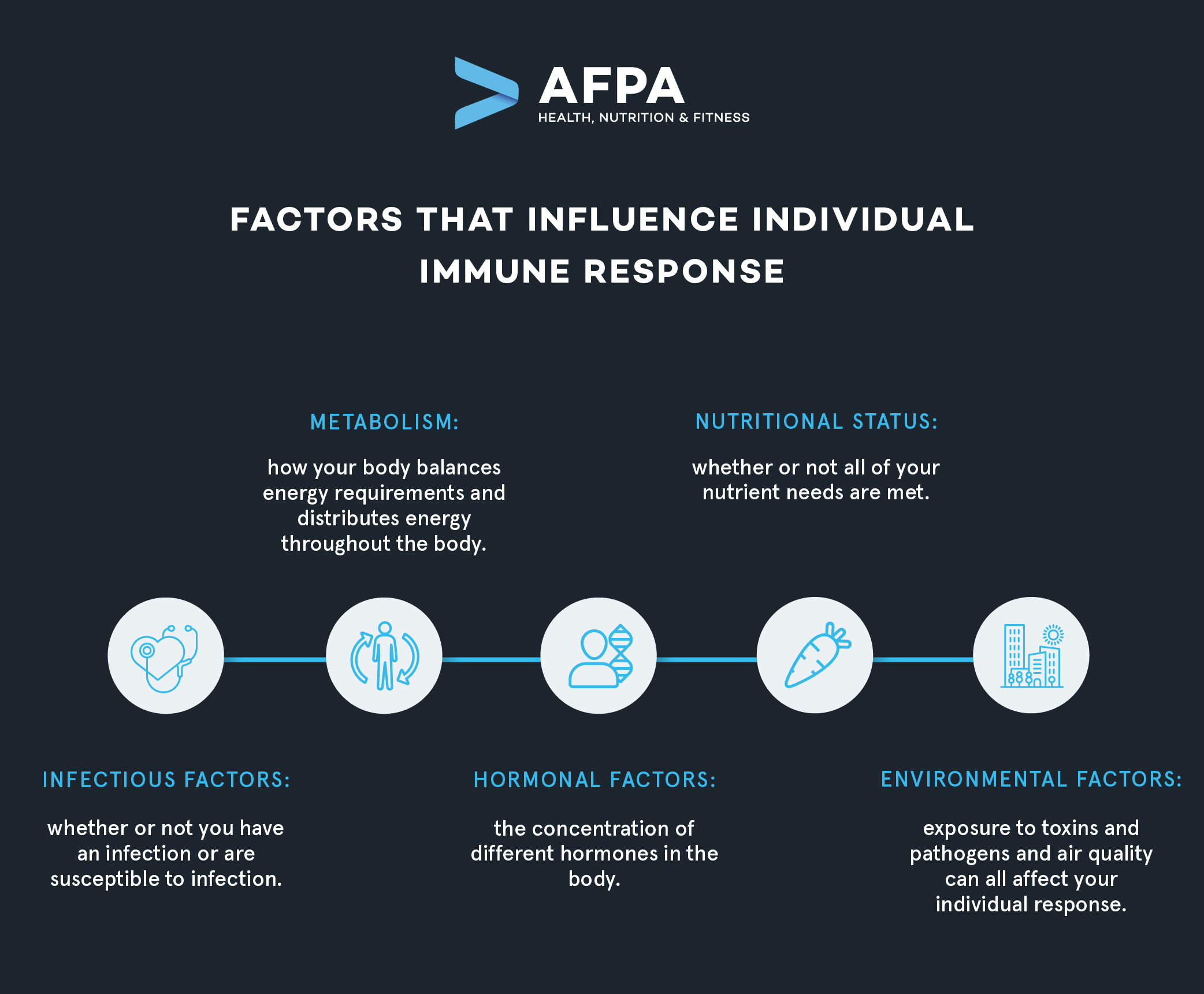
Individual Factors that Impact How Exercise Affects the Immune System
The research we summarize above makes it clear that exercise does affect the immune system, but how it affects the immune system, or whether it helps you fight off disease and illness, depends on multiple individual factors, see below.
Exercise Characteristics that May Affect the Impact on Immunity
There are thousands of exercise variations in terms of activity, intensity, duration, and many other factors.
Research has made clear that the impact exercise has on the immune system depends on a combination of all of these factors, along with the individual factors mentioned above.
Some of the exercise characteristics that impact how your immune system responds include:
- Intensity
- Duration
- Exhaustion levels
- Mode
- Types
For people who are new to exercising, it can be difficult to strike the right balance between the intensity and duration of exercise and the right type of exercise that will meet their needs.
This is where the role of fitness coaches and personal trainers becomes essential to building an effective exercise routine.
Visual Aides: Two Models that Describe Immune Response to Exercise
The research we reference above makes clear that there is not a linear effect of exercise on the immune system. In other words, more intense exercise doesn’t result in better immunity. Researchers have developed two models, the ‘Open Window’ theory and the J-Curve, to describe the immune response to exercise, both of which are illustrated as graphs.
The following tools will help you to apply the research to your own exercise regimen and help you to explain your recommendations to your clients.
The ‘Open Window’ Theory
The “Open Window” theory describes how the immune system is suppressed after high-intensity exercise.
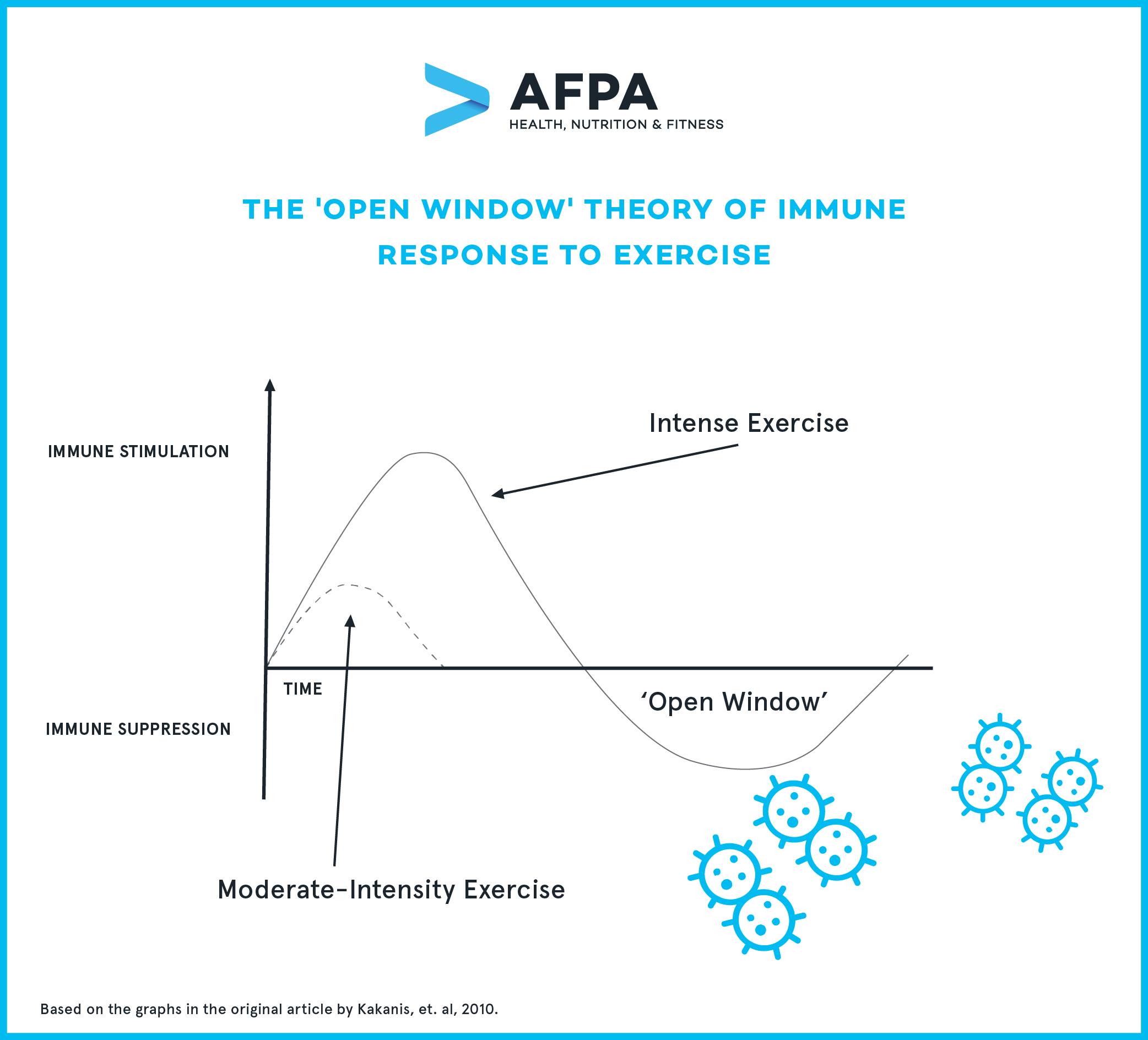 Source: Kakanis, et. al, 2010.
Source: Kakanis, et. al, 2010.
The theory is based on clinical evidence that shows that with intense exercise, like HIIT, sprinting, or similar exercise types, the immune system is boosted significantly, but then suppressed in the 24 hours after exercise. The immune suppression is referred to as the “open window” since it is when your body is more susceptible to pathogens.
What does this mean? When a person performs high-intensity exercise and is exposed to a pathogen in the 24 hours following exercise, they may be more likely to get ill.
However, the immune response is different if you perform moderate exercise. You’ll notice on the curve above that there isn’t immune suppression after moderate-intensity exercise—in fact, the immune system is moderately stimulated.
The ‘J Curve’ Concept
The “J Curve” concept unifies the impact of exercise intensity on the immune system response. The curve demonstrates that people who regularly perform moderate-intensity exercise improve their immune system, but excessive bouts of prolonged training can impair healthy immune function, making people more susceptible to upper respiratory infections.
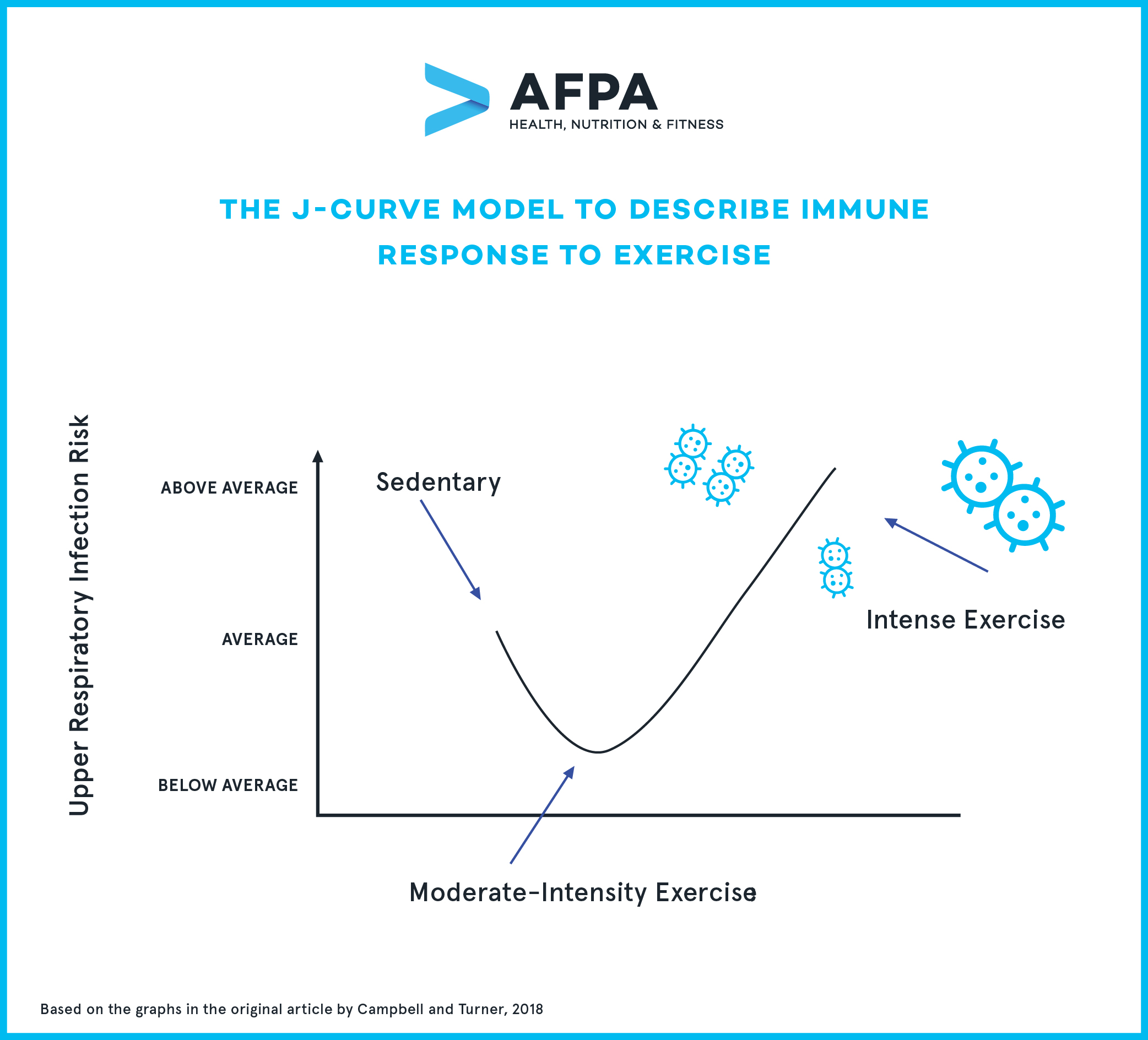 Source: Campbell and Turner, 2018
Source: Campbell and Turner, 2018
As you can see from the graph above, regular moderate-intensity exercise reduces your risk of getting an upper respiratory infection (or other infections, for that matter), while people who perform heavy bouts of intense exercise have even more risk than sedentary people to develop an infection.
This model points to the importance of sticking to a moderate-intensity exercise routine to ensure a healthy immune response.
6 Principles to Follow to Build an Immune-Boosting Exercise Routine
Practice Moderate-Intensity Exercise
If you read the information above, it’s probably clear to you now that all evidence points toward practicing moderate exercise to keep your immune system in tip-top shape.
When you practice moderate-intensity exercise, the immune response is strengthened in many ways:
- You have an enhanced innate immune response.
- You have a reduced risk of chronic disease.
- Your body fights immunosenescence or the effects of aging on immune function.
The evidence about the importance of moderate exercise for the immune system is so strong that researchers are recommending that people who are at risk of being in contact with the coronavirus practice moderate exercise regularly, avoid high-intensity exercise, and even continue to exercise if they have manageable symptoms of COVID-19.
What exactly defines “moderate-intensity” exercise? The Harvard T. Chan School of Public Health defines moderate-intensity activities as those that get you moving fast or strenuously enough to burn off three to six times as much energy per minute as you do when you are sitting quietly.
Another way to determine exercise intensity is by measuring the heart rate. Moderate-intensity exercise will put a person’s heart rate at 50-70% of their maximum heart rate. If you don’t know what your maximum heart rate is, you can refer to the American Heart Association’s heart rate chart.
Have a Post-Exercise Snack
Above, we describe how exercise may spark a stress-response, which in turn can cause a rise in inflammatory markers. Carbohydrate availability helps to attenuate the inflammatory response post-exercise.
Make a complex carbohydrate part of your post-exercise snack to help fight inflammation. Some ideas include a fruit, vegetable, or whole-grain snack.
Do Not Allow Yourself to Get Exhausted During Exercise
The key to determining the correct intensity of exercise to support the immune system is to avoid reaching a point of exhaustion.
Logically, everyone’s body responds to different exercises differently. A person’s fitness level will determine what is considered moderate exercise for different individuals.
If a person feels exhausted during or after exercise, they have gone beyond their target heart rate for moderate exercise (50-70% of your maximum heart rate), and their immune systems will be compromised for at least 24 hours post-exercise.
Gradually Increase Intensity and Duration of Exercise
As your body’s cells and tissues become accustomed to different exercise modes, intensities, and duration, it is important to adjust activity levels.
Anyone who is just starting out an exercise regimen and sticks to it over several weeks and months will notice how exercises that used to make them feel exhausted will soon feel easy. This is because your metabolism is adjusting to new activity levels; in other words, your body’s organs are learning to become more efficient at using energy and making nutrients available.
So, what used to be a moderate-intensity exercise for someone will soon feel too easy, and they will no longer be reaping the benefits of moderate exercise for the immune system.
Work with a fitness coach to reevaluate exercise intensity, duration, and type every two to four weeks to ensure you are continuously, but gradually, improving your fitness level.
Exercise Regularly (for Ever!)
One of the keys to benefitting from the effects of moderate exercise is to make it part of your regular routine. When you are regularly physically active, you have reduced systemic inflammation.
How much exercise should you aim for? The American Heart Association recommends at least 150 minutes of moderate-intensity exercise a week, which is equal to thirty minutes a day, five days a week. However, the AHA points out that you can gain even more health benefits by exercising at a moderate-intensity at least 5 hours a week.
Adjust your exercise intensity and type as you age. If your abilities change due to injury or disability, talk to your physician and a certified fitness coach to find the best way to stay active.
If You Do Intense Exercise, Rest and Recover
High-intensity exercises have benefits for the overall fitness levels of some athletes and people with specific conditions. High-intensity interval training (HIIT), for example, is associated with many cardiovascular and metabolic benefits.
Therefore, it isn’t necessary to stray away from high-intensity exercises if it helps you meet your or your clients’ fitness goals. It is important, however, to give your body time to recover after performing high-intensity exercise, since your immune system will be suppressed for about a day afterward.
Remember that during the period of recovery you are more susceptible to getting ill. For this reason, in addition to withholding from exercise or performing only light exercise, you should also stay at home or use precautions if you have to go out, like wearing a mask and washing your hands frequently.
Main Takeaways
Making exercise part of your lifestyle is essential for fighting chronic diseases. Research also shows that exercise is important for protecting your body against infections and acute illness. However, in order to reap the benefits of exercise for the immune system, it is important to follow a planned and structured exercise routine that is based on your abilities and fitness level.
You can build an immune-strengthening exercise routine for yourself or your clients by making sure that you stick to moderate-level exercises, refuel carbs after exercise, increase exercise intensity as your body becomes accustomed to it, and exercise regularly for the rest of your life.
While there is a consensus among exercise immunologists that moderate-level exercise is best for the immune system, if you do choose to take part in high-intensity exercise, it is important to give your body the rest it needs to recover healthy immune cell levels.
Exercise is an important part of a holistic strategy for strengthening the immune system, so make sure that you follow research-backed principles when building your exercise routine.




